Healthcare White Paper
Enhancing Patient Outcomes and Operational Efficiencies with Hospital Automation for Infection Control
Introduction
Infection control has always been a critical aspect of healthcare, particularly in hospital settings where vulnerable patients are at an elevated risk of healthcare-associated infections (HAIs). The traditional approaches to infection control, heavily reliant on manual processes, not only create substantial workloads for environmental services (EVS) staff but also leave room for inconsistencies and human error. With the rapid advancements in technology, there is a growing trend towards integrating automation into hospital operations to improve infection control and overall healthcare delivery.
The recent COVID-19 pandemic has underscored the urgent need for more efficient and reliable infection control measures. It has exposed the vulnerabilities in current healthcare systems and highlighted the importance of minimizing manual intervention to reduce the spread of infections. Automation, particularly with touchless disinfection systems, offers a promising solution. These systems can significantly reduce HAIs, improve patient outcomes, and enhance operational efficiencies by automating routine tasks, providing real-time monitoring, and enabling rapid, data-driven decision-making.
This paper explores the role of hospital automation within infection control, focusing on how advanced technologies like aerosolized hydrogen peroxide (aHP) and integrated automation can revolutionize infection control practices. It examines the driving forces behind this shift, the economic and social impacts of HAIs, and the potential benefits of adopting automated solutions like the Breezy Platform™. By leveraging these technologies, hospitals can not only enhance patient safety and quality of care, but also achieve significant operational efficiencies and cost savings.
Forces Driving Hospital Automation for Infection Control
Traditional hospital infection control procedures rely heavily upon manual and reactive processes. This can lead to inefficiencies, increased operational costs, and suboptimal patient outcomes. Social, economic, and technological forces are converging to enable rapid innovation in hospital automation for infection control.
-
Social forces: The pandemic exacerbated healthcare labor shortages, and at the same time, exposed the risk of disease spread within healthcare facilities. According to the American Hospital Association, there will be a critical shortage of 3.2 million healthcare workers by 2026 [1].
-
Economic forces: Healthcare-associated infections (HAIs) increase patient stays and expenses, cause staff shortages due to illness, and reduce Medicare/Medicaid reimbursements, stressing a margin-thin industry. According to the U.S. Centers for Disease Control, HAIs have direct medical costs to U.S. hospitals of at least $28.4 billion each year [2].
-
Technological forces: Advances in automation technology enable cost-effective solutions for “touchless” infection control, and those solutions can be leveraged for other hospital applications such as room monitoring, staff workflow optimization, and asset tracking.
The Cost of Healthcare-Associated Infections
The U.S. Centers for Disease Control reports that each day, approximately one in 31 patients in U.S. hospitals contracts at least one HAI [3]. HAIs have direct medical costs of at least $28.4 billion each year, and account for an additional $12.4 billion in costs to society from early deaths and lost productivity [2].
The U.S. Department of Health and Human Services has identified two pathogens, MRSA (methicillin-resistant Staphylococcus aureus) and CDI (Clostridium difficile infection), as top priorities for their HAI National Action Plan [4]. HAIs from these two pathogens are contracted primarily through surface contamination. Microbiologic surveys of hospital rooms of patients with CDI find CDI spores nearly 100% of the time, with toilets, sinks, and high-touch surfaces carrying the highest organism burden [5]. MRSA within a hospital setting is primarily acquired from contact with contaminated items such as instruments, bedding, doors, and equipment [6]. A research paper that reviewed 28 different studies on CDI concluded that patients with hospital-acquired CDI cost healthcare systems an additional $24,000 [7]. A similar study shows that each case of hospital-acquired MRSA increased hospital expenses by $22,293 [8].
In addition to direct medical costs, high HAI rates can affect Medicare fee-for-service reimbursements to hospitals. Hospitals report quarterly on HAIs, and the Centers for Medicare and Medicaid Services (CMS) tracks hospital HAI rates as part of its Hospital-Acquired Condition Reduction Program [9]. CMS sets HAI benchmark targets for all hospitals, including benchmarks for MRSA and CDI occurrences. Under the program, CMS reduces overall Medicare payments by up to 1% for hospitals that rank nationally in the worst-performing quartile on HAI metrics. This CMS program provides significant financial incentives for hospitals to control HAIs.
Supplemental Disinfection with Aerosolized Hydrogen Peroxide
Hand hygiene has long been regarded as a cornerstone of infection prevention, marketed as an inexpensive and effective strategy for reducing the HAIs spread by healthcare workers [10]. A paper compiling 35 hand hygiene studies found that most studies reported hand hygiene compliance rates between 60% and 70% [11]. Whereas handwashing combats one vector of HAI spread, it does not address surface contamination by patients, visitors or by healthcare workers between hand washings. A supplemental surface disinfection regime has been shown to augment hand hygiene practices to reduce HAIs spread by surface contamination [12].
Hydrogen peroxide has long been used as a liquid spray disinfectant. Hydrogen peroxide has strong oxidizing properties that break down membrane lipids, DNA, and other essential cell components of bacteria, viruses, and other microorganisms, rendering them inactive. When aerosolized, hydrogen peroxide undergoes an accelerated oxidation process due to the much greater exposure to surfaces and airborne particles. During the oxidation process, aerosolized hydrogen peroxide (aHP) fully biodegrades into water and oxygen, making aHP non-toxic, residue-free, and environmentally friendly. And because it neutralizes pathogens in a different manner than antibiotics, aHP does not create drug-resistant pathogens.
Aerosolized hydrogen peroxide and hydrogen peroxide vapor have been used for decades for supplemental disinfection within hospitals. A 10-year study found that adding aHP to regular cleaning reduced CDI rates by 41% in hospital settings [13]. Other studies demonstrate the effectiveness of aHP against pathogens such as SARS-CoV-2 [14] and other bacteria and fungi [15].
Comparison of aHP to Other Forms of Supplemental Disinfection
Many hospitals perform supplemental disinfection manually using backpack or hand sprayers and foggers. This manual disinfection is highly laborious, requires PPE, exposes staff to health risks, and often uses disinfectants that leave residues that require additional labor to remove. There is a modernization trend within healthcare to move to touchless systems for supplemental disinfection that use ultraviolet (UV) light, aerosolized hydrogen peroxide (aHP), or hydrogen peroxide vapor (HPV) [16].
UV systems, including both pulsed xenon and UV-C technologies, are regularly used for supplemental disinfection within U.S. hospitals. The main advantage of UV systems is the immediate reentry after treatment and the elimination of any chemical residues. A major disadvantage is limited room coverage due to shadowing, low penetration depth, and the significant drop off in intensity with distance from the light source. For room disinfection, UV system manufacturers recommend exposure times between 10 and 45 minutes at multiple locations within the room [17]. Consequently, most studies show limited pathogen reduction with UV systems when used within a hospital room setting [16].
There are many studies that show far superior coverage and higher germicidal efficacy of aHP/HPV relative to UV systems [16]. Some aHP and HPV systems use pure hydrogen peroxide formulas which leave zero chemical residue because hydrogen peroxide completely biodegrades into water and oxygen. aHP and HPV systems have seen slower adoption within hospitals, primarily due to complicated room sealing requirements, long contact times after application, and complicated setup, use, and maintenance.
A new aHP applicator, Breezy Blue™ is designed to minimize the time needed for environmental service (EVS) staff to perform supplemental disinfection within a hospital environment. Relative to UV and other aHP/HPV systems which add labor, Breezy Blue requires near zero additional EVS labor to perform supplemental disinfection. Breezy Blue will uniformly fill a room for thorough disinfection coverage from a doorway in less than 5 minutes. This aHP disinfection is performed as the last step in the room cleaning process, allowing the EVS staff to immediately move onto their next task. With the door closed, the micron-size droplets will contact all exposed surfaces in the room and completely evaporate within 45 minutes. The Breezy Blue aHP droplets are small enough to float throughout a room for uniform coverage and rapid evaporation, and large enough to be contained within a room without requiring complicated room sealing as is necessary with other aHP/HPV systems.
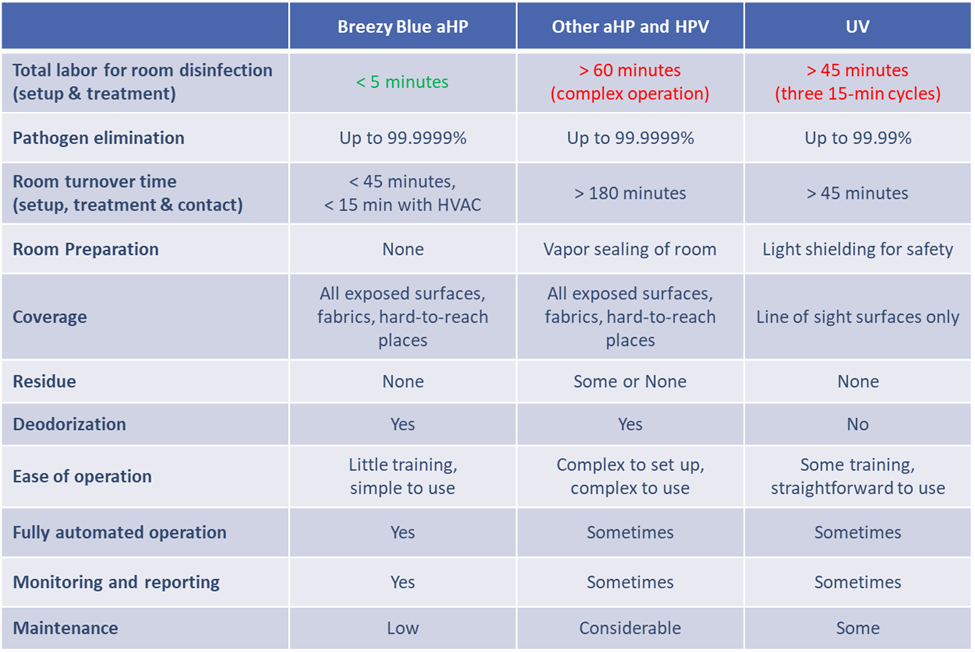
Breezy Blue is an IoT device that is simple to set up and operate, and that has been systematically engineered for an extended maintenance-free service life. Within a hospital environment, Breezy Blue is used as part of terminal cleaning upon room turnover, or automatically overnight in unoccupied rooms such as operating rooms or day clinics. Table 1 compares Breezy Blue to other types of touchless supplemental disinfection. Breezy Blue is part of the Breezy Platform ecosystem of wirelessly connected devices that work collectively to streamline EVS workflows and electronically record supplemental disinfection data for continuous optimization. Other functionalities offered by the Breezy Platform will be described in the following sections of this paper.
The Breezy Platform™: Automating Infection Control
The Breezy Platform is a turnkey hardware and software solution for managing, tracking, and optimizing supplemental disinfection. Figure 1 depicts the various hardware and software components that make up the Breezy Platform, which include Breezy Blue, Breezy Sense™, Breezy Link™, and Breezy Cloud™. Breezy Sense is a real-time aHP sensor to optimize aHP dosage and room reentry. Breezy Sense also measures room occupancy, air quality, and environmental conditions. Breezy Link is a wireless gateway that connects all Breezy devices into the Breezy Cloud, a data warehouse for the Breezy data.
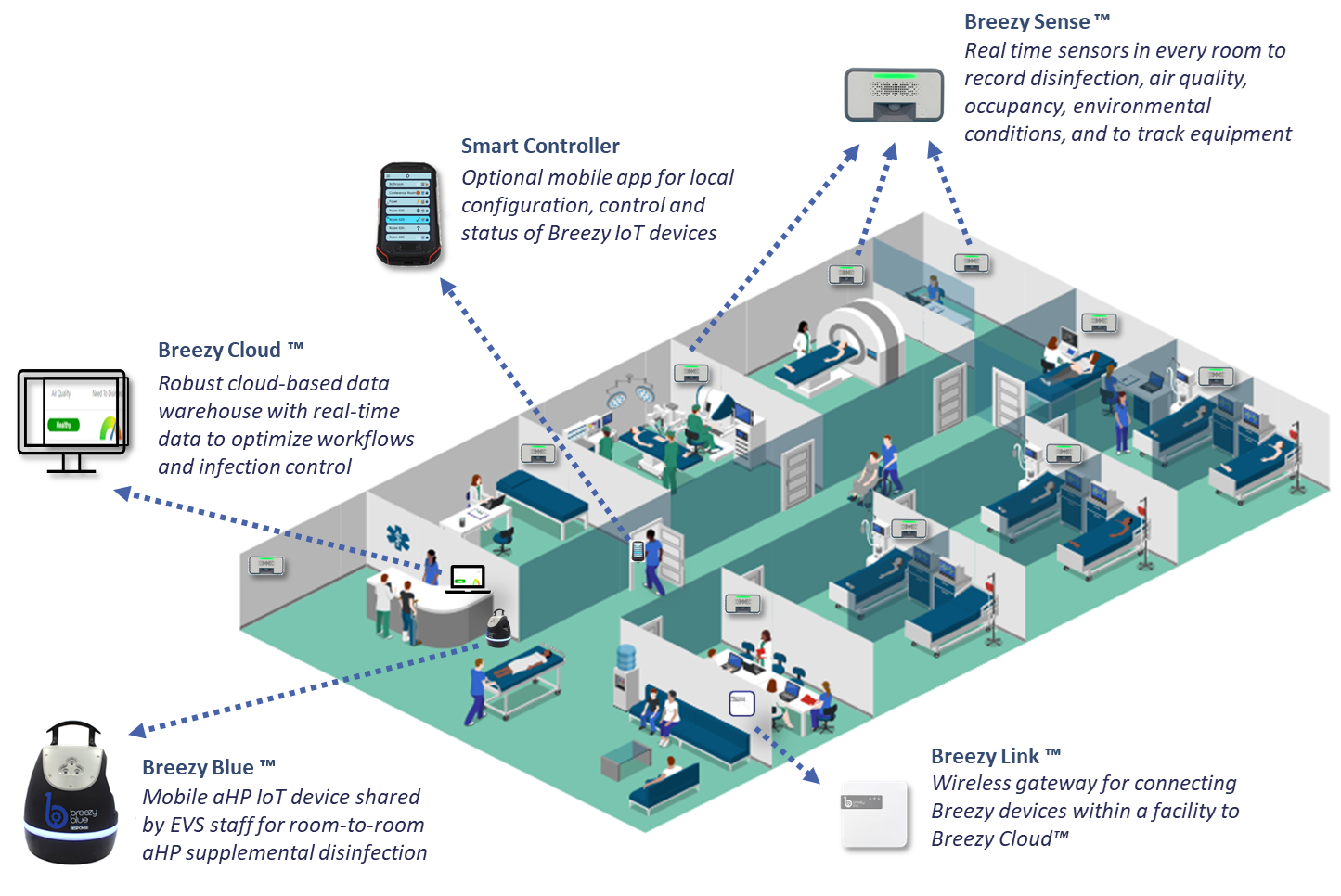
The typical Breezy Platform configuration for a hospital includes the following devices, all of which are provided as a turnkey solution that includes all hardware, software, disinfectant, and service. There is a single monthly charge based on the number of beds in the hospital.
-
One Breezy Sense per hospital room to measure disinfection dosage, air quality, environmental conditions, and occupancy.
-
One Breezy Blue and two gallons/month of Breezy BioCare RTU per hospital wing for thorough supplemental disinfection by EVS staff upon room turnover.
-
One Breezy Link per hospital wing for wireless Bluetooth Low Energy (BLE) coverage.
-
One Breezy Cloud site license per hospital.
Use Case Example
Based upon the national benchmarks, a 200-bed hospital with 50,000 patient days per year will have on average 26 cases of CDI and two cases of MRSA over a 12-month period. Using the research study data cited earlier [7,8], these HAIs will cost the hospital approximately $670,000 in direct healthcare costs. This does not include the impact on payer reimbursement rates nor the financial consequences to society from early deaths and lost productivity.
By reducing HAIs by 41% as shown in the aHP study cited earlier [13], adding aHP supplemental disinfection to this 200-bed hospital will save approximately $274,000 per year. The monthly subscription for the Breezy Platform to provide automated supplemental disinfection with traceable electronic records within a 200-bed hospital would cost $7,500 per month or $90,000 per year. This subscription includes all equipment, all software licenses, and all hydrogen peroxide disinfectant used. This simple investment in automated touchless disinfection solutions will return an immediate 3:1 savings with zero up-front costs. The Breezy Platform automation offers additional functionalities and cost benefits when integrated within a larger hospital internet of things (IoT) ecosystem.
The Breezy Platform within a Hospital IoT Ecosystem
The Breezy Platform uses Bluetooth Low Energy (BLE) wireless connectivity that requires minimal integration and has little impact upon a hospital IT environment. All operational data is secure and does not include any patient or medical information. Data is stored within the Breezy Cloud data warehouse which enables users to view operational dashboards from any location. Also, the Breezy Platform is interoperable with other BLE devices such as BLE beacons and tags for real-time location services (RTLS).
Hospitals are rapidly adopting IoT automation to streamline operations and address labor shortages. Healthcare IoT is predicted to grow at a CAGR of 13.2% to $330 billion in 2027 [18]. Current Hospital IoT applications include asset tracking, bed management, patient monitoring, hand hygiene monitoring, wander management, digital wayfinding, and other similar functions. The Breezy Platform enhances a hospital IoT ecosystem by integrating unique applications such as disinfection management and occupancy-based EVS workflow management. And because there is a Breezy Sense in every room, the Breezy Platform enhances the value of other automated systems with features such as indoor air quality monitoring and environmental monitoring for facility HVAC maintenance and optimization, and room-by-room asset tracking for RTLS systems.
Conclusion
The integration of automation technologies within hospital infection control represents a pivotal advancement in healthcare, offering significant benefits in terms of patient outcomes and operational efficiencies. Traditional infection control measures, while effective, are often labor-intensive, time-consuming, and susceptible to human error. The emergence of automated solutions such as the Breezy Platform, which incorporates touchless supplemental disinfection with aerosolized hydrogen peroxide, exemplifies the transformative potential of modern technology in this domain.
By harnessing the capabilities of IoT devices and real-time monitoring systems, hospitals can streamline disinfection processes, ensure consistent application, and maintain comprehensive records for continuous improvement. The economic impact of reducing healthcare-associated infections is substantial, as demonstrated by the potential cost savings in the use case example for a 200-bed hospital. Moreover, the broader implications of improved patient safety, enhanced hospital reputation, and compliance with regulatory standards underscore the value of adopting such innovative solutions.
The Breezy Platform not only addresses the immediate needs of infection control but also integrates seamlessly into the larger Hospital IoT ecosystem, providing a foundation for further advancements in hospital automation. As the healthcare landscape continues to evolve, the adoption of technologies like those described in this paper will be essential for meeting the challenges of a growing and aging population, managing costs, and maintaining high standards of care.
In conclusion, hospital automation for infection control is no longer a future concept but a present necessity. The deployment of advanced technologies to automate and optimize infection control processes is a crucial step towards a more resilient, efficient, and patient-centric healthcare system. The benefits of such innovations, from cost savings to improved patient outcomes, make a compelling case for their widespread adoption.
For more information
Chris Ziomek, CEO
Build With Robots
info@buildwithrobots.com
833-273-3568
https://buildwithrobots.com/breezy-platform
Copyright 2024 - Build With Robots